Healthcare Data Connectors
Healthcare organisations worldwide face a critical challenge: their systems can’t communicate with each other. If you’re dealing with scattered patient data, expensive vendor API fees, unreliable connections, and manual data entry between systems, you’re not alone. This comprehensive guide explores two distinct healthcare data integration solutions that solve different but equally important problems in modern healthcare IT infrastructure.
The Healthcare Data Integration Crisis {#problem}
Healthcare IT infrastructure is fundamentally broken. According to recent industry studies, the average healthcare organisation uses 15-20 different software systems that rarely communicate effectively with each other. This digital fragmentation creates numerous operational challenges:
Common Healthcare IT Pain Points:
Scattered Systems: Patient data exists in multiple disconnected databases – EMRs, billing platforms, lab systems, imaging systems, and speciality applications operate in isolation.
Expensive Vendor APIs: Major EHR vendors charge $50,000 to $200,000 for basic integration packages, with ongoing licensing fees that can reach 20% annually.
Extended Support Cycles: Simple integration changes often require 3-4 weeks for vendor support teams to implement, disrupting critical workflows.
Unreliable Connections: Custom point-to-point integrations frequently fail, causing data loss and workflow interruptions.
Scalability Issues: Traditional integration approaches break down as data volumes increase or new systems are added.
Compliance Complexity: Each integration must meet HIPAA, HL7, and other healthcare data standards, multiplying development time and costs.
Understanding Healthcare Integration: Two Distinct Solution Categories {#solutions}
Healthcare data integration requirements fall into two primary categories, each requiring specialized approaches:
System-to-System Integration
Connecting healthcare software applications, databases, and cloud platforms for seamless data exchange between administrative and clinical systems.
Device-to-System Integration
Connecting physical medical equipment, lab instruments, and IoT devices to healthcare information systems for automated data collection and processing.
Most healthcare organisations require the first type, with device integration serving as a complementary solution for facilities with automated medical equipment.
Solution 1: System Data Connector for Healthcare Software Integration {#solution1}
What It Does
The System Data Connector specialises in connecting healthcare software applications, enabling seamless data flow between EMRs, billing platforms, patient portals, and external data sources.
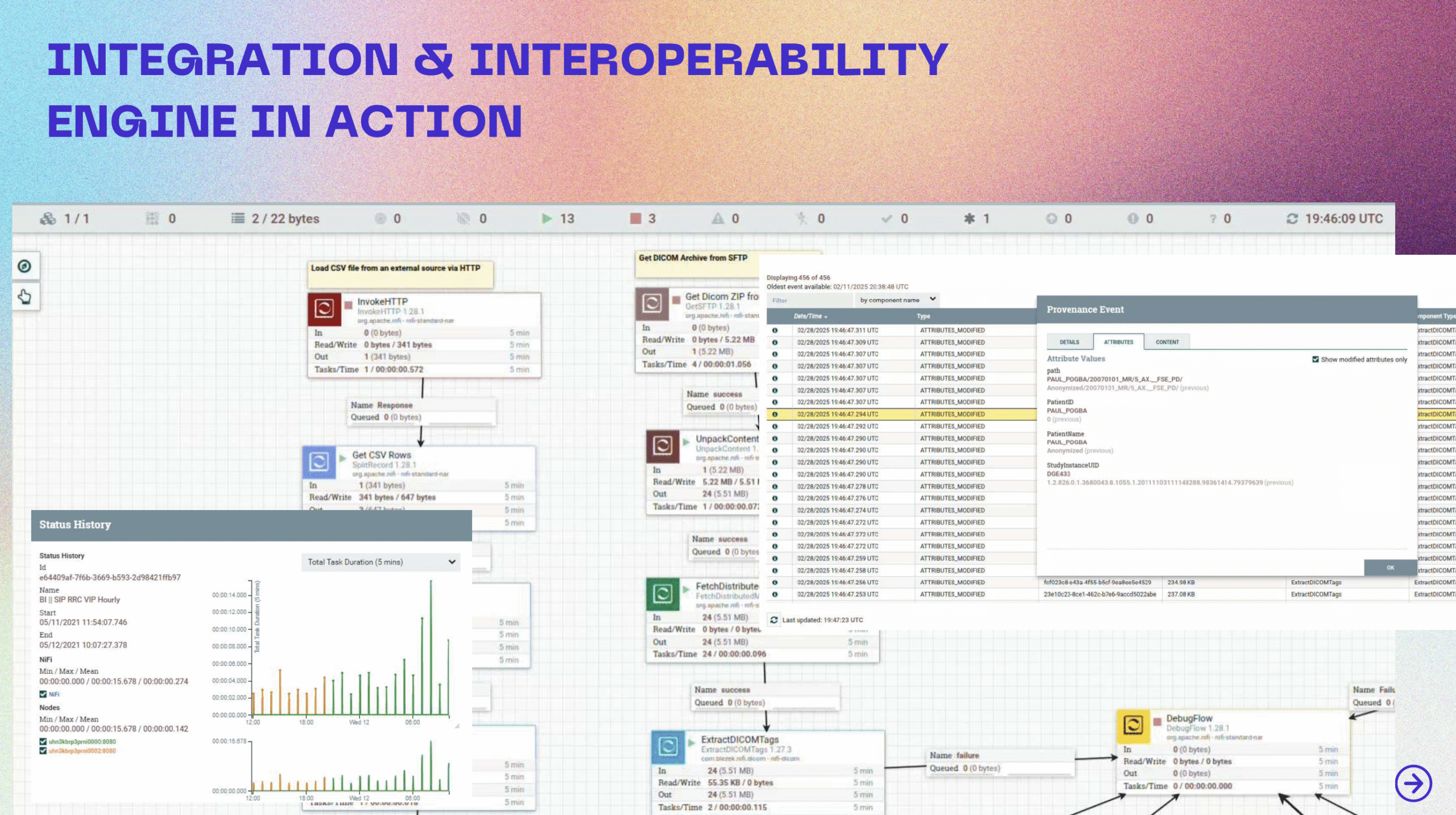
Key Capabilities:
FHIR API Integration: Native support for Fast Healthcare Interoperability Resources (FHIR) R4, STU3, and DSTU2 standards, enabling connections with Epic, Cerner, Allscripts, and other major EHR systems.
Real-Time Data Processing: Processes healthcare data in real-time rather than batch operations, ensuring clinical staff always have access to current patient information.
Data Transformation: Automatically converts data between different formats and standards, eliminating the need for custom middleware development.
Audit Trail Management: Maintains comprehensive logs of all data transactions for HIPAA compliance and regulatory reporting.
Error Handling and Recovery: Built-in mechanisms to detect, report, and recover from integration failures without manual intervention.
Supported Integration Types:
- EMR to EMR data exchange
- Billing system integration
- Patient portal data feeds
- Insurance verification workflows
- Clinical data repository connections
- Reporting and analytics system feeds
- Telehealth platform integration
- Third-party application connections
Epic EHR Integration: A Detailed Case Study
Epic Systems dominates the EHR market with approximately 34% market share in the United States. However, Epic’s premium integration packages often cost $75,000+ with ongoing licensing fees.
The USCDI on FHIR Advantage
Epic provides free access to patient data through their United States Core Data for Interoperability (USCDI) on FHIR API. This regulatory requirement, stemming from the 21st Century Cures Act, mandates that EHR vendors provide standardized API access to core patient data elements.
Available Data Types Through Epic’s Free USCDI API:
- Patient demographics and contact information
- Problem lists and medical conditions
- Medication lists and prescriptions
- Laboratory results and diagnostic reports
- Clinical notes and documentation
- Vital signs and observations
- Immunization records
- Allergy and intolerance information
- Procedure history
- Care team information
Implementation Process:
- Registration: Create a free developer account at uscdi.epic.com
- API Access: Review available endpoints and data specifications
- Authentication: Implement OAuth 2.0 with PKCE for secure access
- Data Mapping: Configure field mappings between source and target systems
- Testing: Validate data flow using Epic’s sandbox environment
- Deployment: Launch integration with real-time monitoring
Solution 2: Medical Device Connector for Equipment Integration {#solution2}
What It Does
The Medical Device Connector specialises in bidirectional communication between medical equipment and healthcare information systems, automating data collection and result processing.
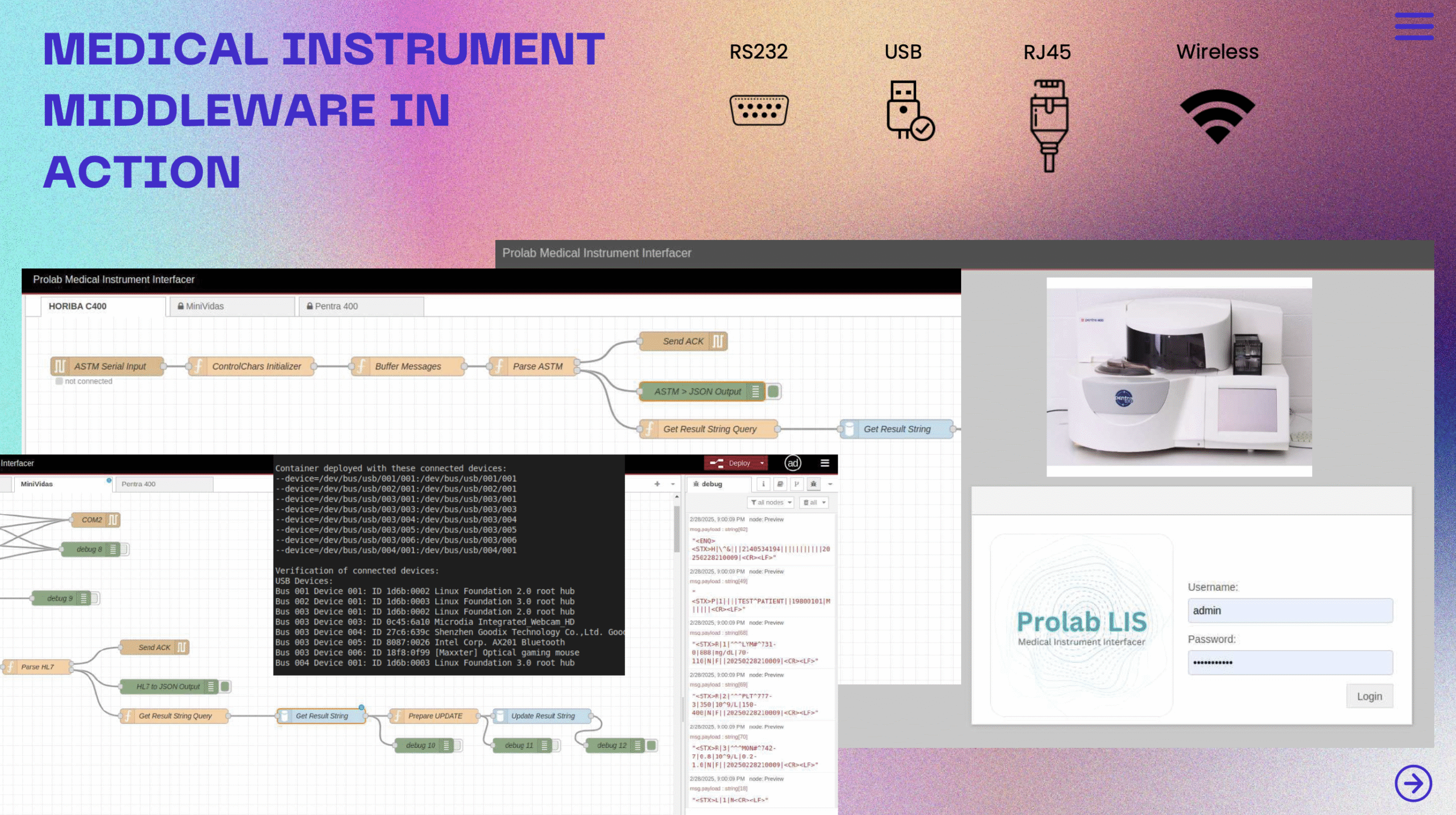
Key Capabilities:
Protocol Translation: Supports multiple communication protocols including HL7 v2.x, ASTM, and proprietary instrument protocols.
Bidirectional Communication: Sends test orders to instruments and receives results automatically, eliminating manual data entry.
Real-Time Processing: Processes instrument data immediately upon receipt, reducing result reporting times from hours to minutes.
Quality Control: Validates instrument data for accuracy and completeness before forwarding to laboratory information systems.
Status Monitoring: Tracks instrument connectivity, performance, and error conditions in real-time.
Supported Device Categories:
- Laboratory analyzers (chemistry, hematology, immunology)
- Imaging equipment (X-ray, MRI, CT scanners)
- Patient monitoring devices (vital sign monitors, telemetry)
- Point-of-care testing devices
- Infusion pumps and medication dispensers
- Pathology equipment (microscopy, tissue processors)
Real-World Implementation Examples {#examples}
Case Study 1: Epic EMR Integration Without Premium Costs
Client: Mid-sized hospital system with 200 beds Challenge: Integrate external FHIR patient data and Sage billing information with Epic EMR Previous Solution Cost: Epic quoted $75,000 for integration package plus 20% annual maintenance
Implementation Approach:
- Utilized Epic’s free USCDI on FHIR API endpoints
- Built data transformation pipelines for external FHIR to Epic format conversion
- Created automated billing data mapping from Sage to Epic’s financial modules
- Implemented OAuth 2.0 authentication with PKCE for mobile security
- Set up real-time monitoring dashboard with error alerting
Results Achieved:
- Zero ongoing API licensing costs
- Real-time data synchronization replacing nightly batch processes
- Complete audit trail for regulatory compliance
- 10x scalability without additional vendor fees
- 3-week implementation vs. 6-month vendor timeline
- $180,000 total cost savings over three years
Technical Benefits:
- Access to all USCDI-mandated data elements
- Standardized FHIR R4 data format
- OAuth 2.0 security compliance
- Automated error handling and retry logic
- Performance monitoring and alerting
Case Study 2: Laboratory Instrument Integration
Client: Regional diagnostic laboratory processing 5,000 tests daily Challenge: Connect Prolab LIS with four different analyzer types Equipment: Pentra (chemistry), Horiba (hematology), Sysmex (cell counting), Tosoh (immunoassay)
Implementation Approach:
- Built custom protocol adapters for each instrument type
- Created unified data translation layer for result standardization
- Implemented bidirectional order/result workflow
- Set up real-time instrument status monitoring
- Added automated quality control validation
Results Achieved:
- 90% reduction in manual data entry
- Result reporting time: 45 minutes → 3 minutes
- Unified technician interface for all instruments
- 24/7 automated operation with error alerting
- 99.7% data accuracy with automated validation
- $120,000 annual labor cost savings
Operational Benefits:
- Simultaneous order distribution to multiple instruments
- Automatic result validation and quality control
- Real-time instrument status monitoring
- Centralized error handling and troubleshooting
- Comprehensive audit trail for laboratory accreditation
Healthcare Integration Cost Analysis and ROI {#cost}
Traditional Vendor Integration Costs:
Initial Implementation:
- Epic integration package: $75,000 – $150,000
- Cerner integration: $50,000 – $125,000
- Custom development: $100,000 – $300,000
- Project management: $25,000 – $75,000
- Total: $250,000 – $650,000
Ongoing Costs (Annual):
- Vendor maintenance fees: 18-22% of initial cost
- Support and updates: $15,000 – $45,000
- Additional user licenses: $5,000 – $25,000
- Total Annual: $60,000 – $180,000
Our Integration Solution Costs:
System Data Connector:
- Implementation: $25,000 – $75,000
- Configuration and testing: $10,000 – $25,000
- Training and documentation: $5,000 – $15,000
- Total: $40,000 – $115,000
Medical Device Connector (Add-on):
- Implementation: $15,000 – $35,000
- Device-specific adapters: $3,000 – $8,000 per device type
- Total: $18,000 – $50,000
Annual Maintenance:
- Support and updates: $8,000 – $20,000
- Monitoring and optimization: $3,000 – $10,000
- Total Annual: $11,000 – $30,000
ROI Calculation:
Three-Year Cost Comparison:
- Traditional vendor solution: $430,000 – $1,190,000
- Our integration solution: $73,000 – $205,000
- Total Savings: $357,000 – $985,000
- ROI: 490% – 480%
Decision Framework: Which Solution Do You Need? {#decision}
Start with System Data Connector if you have:
✅ Multiple software systems that don’t communicate ✅ Manual data entry between healthcare applications ✅ Expensive vendor API fees for basic integrations ✅ Slow, unreliable data exchanges between systems ✅ EMR and billing system connection requirements ✅ Patient portal integration needs ✅ Regulatory reporting challenges ✅ Telehealth platform connectivity requirements
Add Medical Device Connector only if you also have:
✅ Laboratory instruments generating automated results ✅ Medical devices requiring data automation ✅ Equipment data trapped in isolated systems ✅ Manual result transcription workflows ✅ Point-of-care testing devices ✅ Patient monitoring equipment with data output capabilities
Assessment Questions:
- How many software systems does your organization currently use?
- What percentage of your data entry is currently manual?
- How much are you paying for vendor API access annually?
- How long do integration changes typically take to implement?
- Do you have medical equipment that generates data automatically?
Implementation Timeline and Process {#timeline}
System Data Connector Implementation:
Week 1-2: Discovery and Planning
- System inventory and data flow mapping
- Integration requirements gathering
- Security and compliance review
- Technical architecture design
Week 3-4: Development and Configuration
- API endpoint configuration
- Data transformation rule development
- Authentication and security implementation
- Error handling and monitoring setup
Week 5-6: Testing and Validation
- Unit testing of individual integrations
- End-to-end workflow testing
- Performance and load testing
- Security vulnerability assessment
Week 7-8: Deployment and Training
- Production deployment
- User training and documentation
- Monitoring dashboard configuration
- Go-live support and optimization
Medical Device Connector Implementation:
Week 1: Equipment Assessment
- Device inventory and protocol analysis
- Communication interface evaluation
- Data format and timing requirements
- Integration point identification
Week 2-3: Adapter Development
- Protocol-specific adapter creation
- Bidirectional communication setup
- Data validation rule implementation
- Error handling and recovery mechanisms
Week 4: Testing and Validation
- Individual device testing
- Workflow integration testing
- Performance optimization
- Quality control validation
Week 5: Deployment and Training
- Production installation
- Technician training
- Monitoring setup
- Operational handover
Security and Compliance in Healthcare Integration {#security}
HIPAA Compliance Requirements:
Administrative Safeguards:
- Role-based access controls
- User authentication and authorization
- Audit log management
- Incident response procedures
Physical Safeguards:
- Secure server environments
- Workstation security controls
- Device and media controls
- Facility access restrictions
Technical Safeguards:
- End-to-end encryption (AES-256)
- Transmission security (TLS 1.3)
- Access control mechanisms
- Audit trail generation
Industry Standards Compliance:
HL7 FHIR Standards:
- R4 specification compliance
- Resource validation
- Terminology binding
- Search parameter support
OAuth 2.0 Security:
- PKCE implementation for mobile apps
- Scope-based access control
- Token lifecycle management
- Refresh token rotation
Data Encryption:
- Encryption at rest (database level)
- Encryption in transit (API communications)
- Key management and rotation
- Certificate lifecycle management
Audit and Monitoring:
Real-Time Monitoring:
- Data flow performance metrics
- Error rate tracking
- System availability monitoring
- Security event detection
Compliance Reporting:
- HIPAA audit trail generation
- Access log reporting
- Data usage analytics
- Incident tracking and reporting
Frequently Asked Questions
Q: How long does implementation typically take?
A: System Data Connector implementations typically complete in 4-8 weeks. Medical Device Connector add-ons require an additional 3-5 weeks depending on the number and complexity of devices.
Q: What ongoing maintenance is required?
A: Our solutions include automated monitoring, error handling, and self-healing capabilities. Typical maintenance involves quarterly updates and annual compliance reviews.
Q: Can you integrate with our existing EHR system?
A: Yes, we support integration with all major EHR systems including Epic, Cerner, Allscripts, athenahealth, and eClinicalWorks through standardized FHIR APIs and HL7 messaging.
Q: What about data security and HIPAA compliance?
A: All integrations include built-in HIPAA compliance features including end-to-end encryption, audit trails, role-based access controls, and regular security assessments.
Q: How do costs compare to vendor solutions?
A: Our solutions typically cost 60-80% less than traditional vendor integrations while providing faster implementation and greater flexibility.
Conclusion: Transform Your Healthcare Data Integration Strategy {#conclusion}
Healthcare organizations can no longer afford the operational inefficiencies and excessive costs associated with traditional vendor integrations. The combination of regulatory requirements for data interoperability and advances in integration technology creates unprecedented opportunities for cost-effective, rapid implementation of healthcare data connections.
Key Takeaways:
- Start with System Integration: Most healthcare organizations benefit immediately from connecting their existing software systems through our System Data Connector.
- Add Device Integration Selectively: Medical Device Connector functionality should only be added when you have automated medical equipment requiring integration.
- Leverage Free APIs: Epic’s USCDI on FHIR and similar regulatory requirements provide free access to essential patient data, eliminating expensive vendor licensing fees.
- Prioritize Speed and Flexibility: Deploy integrations in weeks rather than months while maintaining full control over your data connections.
- Focus on ROI: Typical implementations achieve 400-500% ROI within three years through reduced vendor costs and operational efficiencies.
Ready to Get Started?
Transform your healthcare data integration strategy with proven solutions that deliver results in weeks, not months. Whether you need to connect software systems, integrate medical devices, or both, we can demonstrate working integrations customized for your specific environment.
Schedule a 48-hour proof-of-concept demonstration to see exactly how these solutions work with your existing systems and data flows